LIFESTYLE SERIES
Fatigue
What is Fatigue?
Fatigue describes the feeling of constant tiredness and weakness which can be physical, mental, or a combination of both. It generally occurs due to a depletion of energy after extensive physical or mental exertion, which often requires time and energy to recover from. In a research study conducted in 2019, it was found that fatigue affects up to 8% of healthy adults.
Fatigue can be very debilitating and frustrating. Malaise and fatigue have commonly been associated with PID (IDF Patient and Family Handbook, 2013). IDFA members have described their fatigue using words such as: ‘Zombie Like’, ‘Brain Fog’ and ‘Weighed Down’.
An understanding of your own fatigue symptoms will help you to manage and cope with your fatigue. Below are some more examples of how members describe their fatigue:
- Heavy
- Memory loss
- Body feels like it’s made of concrete
- Too tired to think
- Battery only ever half full
- Weight on shoulders
- Everything just slows down

PID & Fatigue
People with primary immunodeficiency (PID) often report fatigue, yet this symptom has not been extensively studied in PID. Fatigue is present both before and after the diagnosis in many patients of PID and is described as a feeling of physical and mental exhaustion and therefore an extreme burden on daily life. Most patients of PID say that they sleep very well but remain tired.
Using retrospective data collected from the US Immunodeficiency Network (USIDNET) patient registry, it has been estimated that the prevalence of fatigue among adults with PID is 18%, compared to 6–7.5% in the general population.
Lifestyle
Finding a balance between everyday life and managing fatigue can be difficult. You may have to make changes in your life. It’s important to remember you are more than just your illness and you have a lot to offer this world. Changing your life to manage your fatigue is not giving in to being a ‘sick person’, it’s acceptance of what is happening to your body and finding ways to make things easier for yourself!
“How much is illness and how much is lifestyle?”
This is where self-management comes into play. Many people with PID have other health issues as well – such as allergies, gastrointestinal issues, respiratory problems, migraines, autoimmune illness, and many more! Knowing what’s going on in your body is key to separating illness VS lifestyle fatigue symptoms.
Many IDFA members with PID experience varying levels of fatigue. “Infections are the hallmark of a PID” (IDF Patient and Family Handbook, 2013), and fighting off infections will cause fatigue. It is always important to keep on top of your regular treatments for PID (e.g., IVIg, SCIg, gamma interferon) to reduce your risk of infection.
“Sometimes, with PID, there’s just so much going on in your body it just can’t keep up with it all”
– IDFA Member


Managing & Coping with Fatigue
In speaking to our members, we’ve detailed some of the ways they cope and manage fatigue. We hope you find these member stories, experiences and suggestions helpful in managing and coping with your fatigue.
Pacing
Pacing yourself is a great way to preserve energy and reduce the risk of burnout from pushing yourself. One member describes pacing perfectly: “Instead of gardening all day without a break and feeling exhausted the next day, I do half an hour, then come back inside and rest for half an hour, then go back out again and repeat.”
Pacing can be frustrating at first, especially when you just ‘want to get things done’ or use the excuse “but I have energy now and I might not have any tomorrow!”, however pushing yourself too hard puts you at risk of crashing down and taking longer to build your energy back up.
“You have to ask others to work within your time. Putting limits and boundaries really helps with managing fatigue.”
– IDFA Member
The Spoon Theory
People often remind each other that “we are not our disease” and that is true. However, Spoon Theory allows us to make that separation intellectually.
The Spoon Theory describes the idea of limited energy by using spoons. Energy for people with chronic diseases and PID’s is often limited and depends on many factors such as stress levels, sleep quality and pain. All of these contribute to immunodeficient related fatigue. In the proposed theory, each spoon represents a finite unit of energy. Each day has a finite quantity of spoons and each spoon is taken away as the day progresses.
As the day progresses, you would take each spoon of energy utilised out of the finite quantity. This would enable someone struggling with fatigue to plan out their day without exhausting themselves and take out or add spoons for the next day to better manage their fatigue day by day.
This depiction of finite energy is a simple yet perfect description of how and why people with fatigue must pace themselves and can’t participate in activities like most people can.
While the Spoon Theory is often applied to help outsiders understand what it’s like to live with illness, it helps patients in incredible ways too. It gives you the ability to connect with others, express yourself and work on self-compassion.
Resting
Usually, PID and SID related fatigue is not completely relieved by rest and remains persistent. Resting, together with pacing, is crucial to fatigue management. When you take a break and rest properly, you help recharge your batteries so you can keep going. Planning rest times throughout the day can help with the management of fatigue.
Resting includes having a tea break, laying down or sitting in a comfortable position for a time, trying not to think of anything for a few minutes or being too stimulated. In this busy world, we can feel guilty when resting. It’s important to remind yourself that as part of self-management of fatigue, resting will help in the long run. When you go to take your rest break, take a deep breath, and remind yourself “it’s OK to rest”.
You may need to rest several times a day. Planning rest periods is a great way to keep yourself in a routine and help with day-to-day life activities. Sometimes, you may be so fatigued you need to sleep in your rest periods.
Sleep
Sleep quality has commonly been associated with fatigue in immunodeficient related fatigue. Sleep quality moderates the relationship between fatigue patterns and psychological factors, including depression and anxiety.
We all know how important sleep is but getting the mind to turn off at the end of the day and drift merrily off to sleep is often not as easy as it seems. Patients with PID have discussed frustration towards being fatigued throughout the day and having trouble sleeping at night.
“Sometimes after a long night of sleep, I still feel too tired to get on my feet.”
– IDFA Member
Sleep Hygiene
Practicing good sleeping habits is known as sleep hygiene. These habits include getting up at the same time every day, avoiding caffeine and heavy meals before bedtime, reducing the number of naps during the day and practicing relaxation techniques. Erratic sleep patterns have been shown to have negative effects on the immune system (IDF Patient and Family Handbook, 2013).
Avoiding sleeping during the day will allow you to get more restful sleep during the night, however, you may be so fatigued that staying awake isn’t an option. If this is the case, try limiting your nap to under an hour. Occasionally, if you end up sleeping the whole way through until the next day, don’t be unkind to yourself – it could be what your body needs. Of course, if this is happening on a regular basis you should consult with your health care professional.
Sometimes, the longer it takes to get to sleep, the more frustrated you become as you know it will impact your fatigue levels the next day. Instead of letting this frustration impact your sleep further. if you can’t fall asleep within a reasonable amount of time, get up and start your ‘wind down process’ again. This could include reading a book or having a warm drink.
Member Tips to get a good night's sleep
- Warm milk (with honey!)
- Have a relaxing bath
- Rain app on phone
- Soft music or white noise
- No caffeine after lunch!
- Humidifiers
- Bedroom is clean and comfortable
- Calming tea (like camomile or lavender)
- Breathing exercises
- Heat/cold packs
Exercise
It is important to try and get some gentle exercises in your routine 3-4 times a week. People often experience discomfort and a feeling of ‘stiffness’ when they don’t get out there and get moving. Some people who are very fatigued must start as slow as walking 10-30 metres once a day, have a rest day and then gradually increase the distance bit by bit (pacing).
IDFA members with fatigue have benefited from exercises like:
- Yoga
- Physiotherapy exercises
- Swimming
- Pilates
- Tai Chi
- Walking
- Stretching
- Light weights
These exercises are low impact and a great way to start exercising on a low scale if you suffer from fatigue.
It is important to note that some kinds of exercise may be inappropriate for people with specific PIDs. For example, a boy with Wiskott-Aldrich Syndrome who has a low platelet count should not engage in contact sports. Similarly, people with Chronic Granulomatous Disease should not swim in the ocean or freshwater (IDF Patient and Family Handbook, 2013). Your immunologist can recommend appropriate types of exercise for you if you are unsure.
Pain
Some people experience aches and pains, headaches, and/or a general feeling of heaviness or being weighed down. Depending on the level of pain, it can be very distressing. Fatigue has commonly been identified as a measure of pain. This is because the body requires more energy and focus to utilise the parts of the body that are in pain, which increases physical and mental fatigue.
The overall aim when managing pain is to:
- Minimise inflammation and the perception of pain
- Minimise fatigue
Pain is a dynamic process involving:
- Pain transmission: Neural signals from pain sight up to the brain
- Pain inhibition: Neural signals from brain down to pain site
- Pain perception: The experience of pain as the messages reaches consciousness
Pain Intensity
There are many factors that can also impact pain intensity. These vary widely from person to person, they can include:
- States of excitement, stress or anxiety
- Exposure to others pain
- Past pain experience and anticipation
- Underlying disorders such as anxiety, depression, hyperactivity disorder or autism
- Cultural norms and societal expectations
- Coping ability and style
Member Tips for managing pain
- Heat/cold packs
- Hot shower/bath
- Physiotherapy/osteopathy
- Talking to a therapist (for example psychological, music, art or hypnotherapy)
- Acupuncture and massage
- Meditation
- Hobbies (drawing, knitting)
- Listening to music
- Painkillers (consult with your GP or healthcare professional)
Healthy Eating
A wide variety of nutrient dense foods should be consumed each day to support overall health and wellbeing, the quality of life and reduce the risk of chronic diseases. It is a vital part of the management of fatigue and it can be useful to check with your healthcare provider whether you have allergic reactions to certain foods that might aggravate fatigue.
The immune system is a complex system of organs and processes that actively fights against infections invading the body. Adequate and appropriate nutrition intake is required for all cells within the body to function optimally, including the immune system.
The main macronutrients that the body requires through dietary sources are protein, carbohydrates, dietary fibre and dietary fats.
“Protein is necessary for internal healing as well as energy.”
– IDFA Member
It is also essential to be drinking enough water each day, where women should have around 2 litres or 8 cups, and men have about 2.6 litres or 10 cups per day. (IDFA Nutrition Booklet, 2021)
Choosing the right food to include in your diet is important in optimising mental health and mood. Eating for good gut health, consuming plenty of oily fish, keeping blood sugar levels steady, limiting highly processed and high sugar foods and drinks are a few of the food choices you can make to your diet to protect your mental health, while also ensuring you get plenty of sleep, regular exercise and managing stress effectively.
Member Tips for healthy eating
- Keep easy snacks in the pantry – like rice crackers and tuna, healthy frozen meals
- Cook meals on ‘good days’ and store in the freezer (like soup!) for the ‘not so good’ days
- See if it’s possible to get the groceries delivered
- Ask friends and family or a carer to help out
- Pre-boil eggs as an easy snack in fridge
- Use more Lite ‘n’ Easy or pre-made, aka healthier, store-bought meals
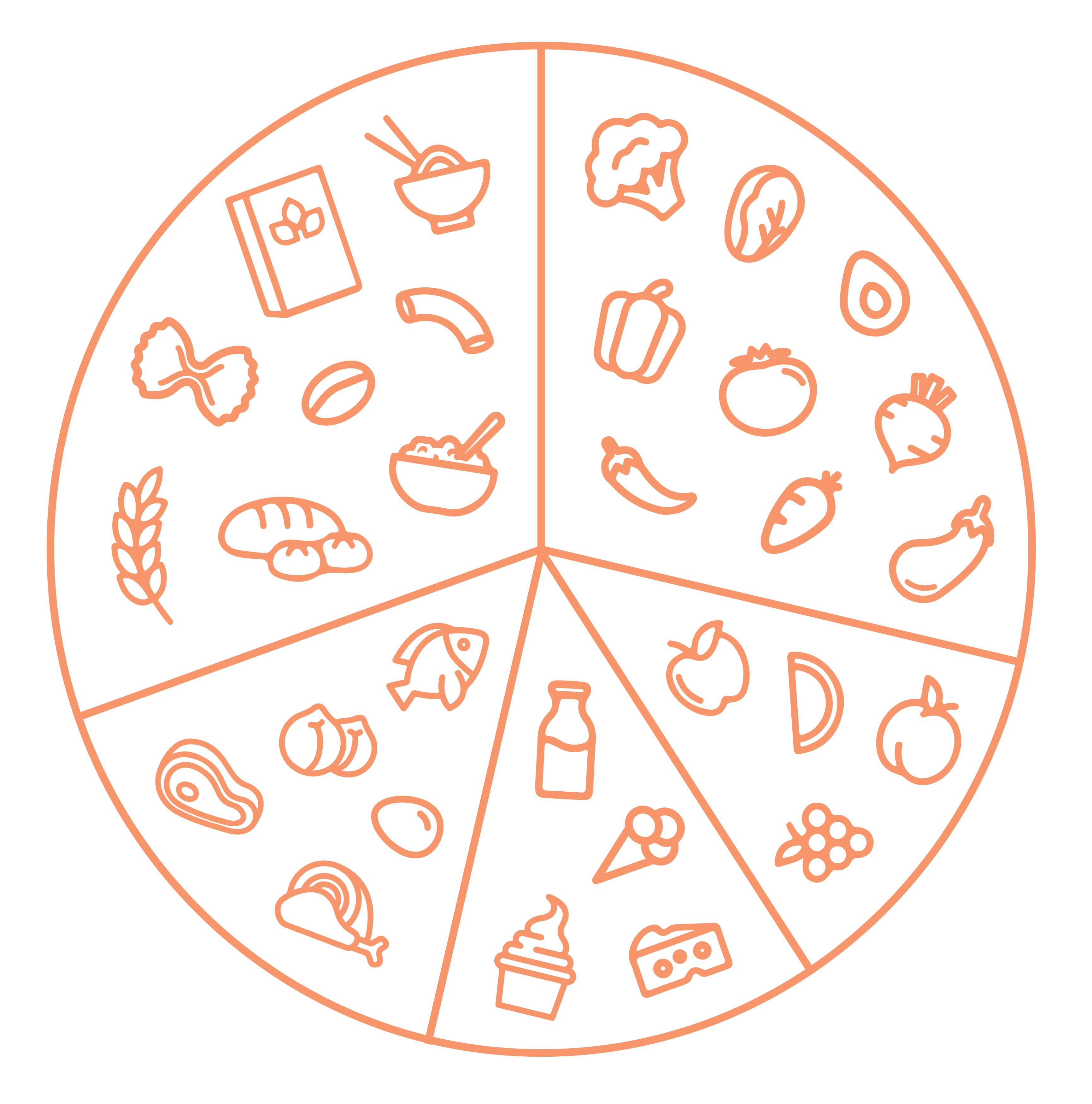
Enjoy a wide variety of nutritious foods from these five food groups everyday.
Graphic adapted from ‘Australian Guide to Healthy Eating’, Eat for Health.
Mental Wellbeing
Keeping on top of any emotional or mental stressors in your life, in addition to resting and eating healthy can help with fatigue management. Sometimes, people may experience fatigue because of depression, extreme stress, anxiety, or other mental illnesses.
“You feel concerned for family members, especially kids, and what they might be thinking or experiencing. It creates a guilt complex with the effect it has on one’s family. But letting them do things for you is okay. They know what you are going through.”
– IDFA Member
Member Tips for stress management
- Self-care
- Acceptance
- Write down thoughts in a thought journal
- Express yourself on IDFA Facebook page
- Mindfulness
- Reach out to support groups
- Breathing exercises
- Meditation and relaxation
- Speak to a close friend or a family member
- Have a cry, let it out
- Go for a walk to clear your mind
- Speak to a counsellor or psychologist
Stigma & PID
Although the research and awareness towards immunodeficiencies has been increasing in recent years, immunodeficiency related fatigue has still not been extensively researched.
Fatigue is not included as a major indicator of immunodeficiency amongst symptoms such as recurrent fevers, eczema, unnatural or weak responses to infections and granulomas. The lack of immunodeficiency related fatigue research makes stigma related to fatigue especially prominent. This can be mentally, physically, and emotionally exhausting for people seeking support related to managing and understanding their immunodeficiency related fatigue.
“[Due to the stigma around fatigue] sometimes you think the fatigue is all in your head. You question why you are tired all the time and become confused. You learn to hide it very well.”
– IDFA Member
As someone with PID, your energy is precious to you. It is not worth spending it on ignorant people, so take a deep breath and let it go. Re-focus your energy away from sources of stigma and prioritise it!
Speak to someone who understands, reach out to support groups, talk to other IDFA members. It can be very difficult when someone close to you does not understand and makes unfair judgements about you.
And always remember, YOU ARE NOT ALONE.
What is Stigma?
Sometimes, you may come across people who do not understand what you are going through. They may make insensitive remarks such as ‘you are just lazy’. This is called stigma.
Stigma is a mark of disgrace that sets a person apart. When a person is labelled by their illness they are seen as part of a stereotyped group. Negative attitudes create prejudice which leads to negative actions and discrimination.
Member Tips for dealing with stigma
- Use IDFA pamphlets to help you cope with and explain symptoms of PID
- Communicate your feelings with the people who matter to you and let them know what to expect from you if you can
- Use methods like spoon theory to explain how you are doing the best you can under the circumstances
IDFA would like to thank its members and Megha Parmar who have contributed to this Lifestyle Series content.

This Lifestyle Series is supported by an unconditional educational grant from Takeda. Takeda has not determined and is not responsible for the content of this pamphlet.











