Advocacy

Driving change by advocating on issues important to Australians living with an immunodeficiency.
We advocate and support research into a range of issues significant to patients with primary and secondary immunodeficiencies. Find out more about our current advocacy initiatives below.
SCID Newborn Screening
Advocating for the routine implementation of SCID (Severe Combined Immunodeficiency) Newborn Screening Australia-wide.
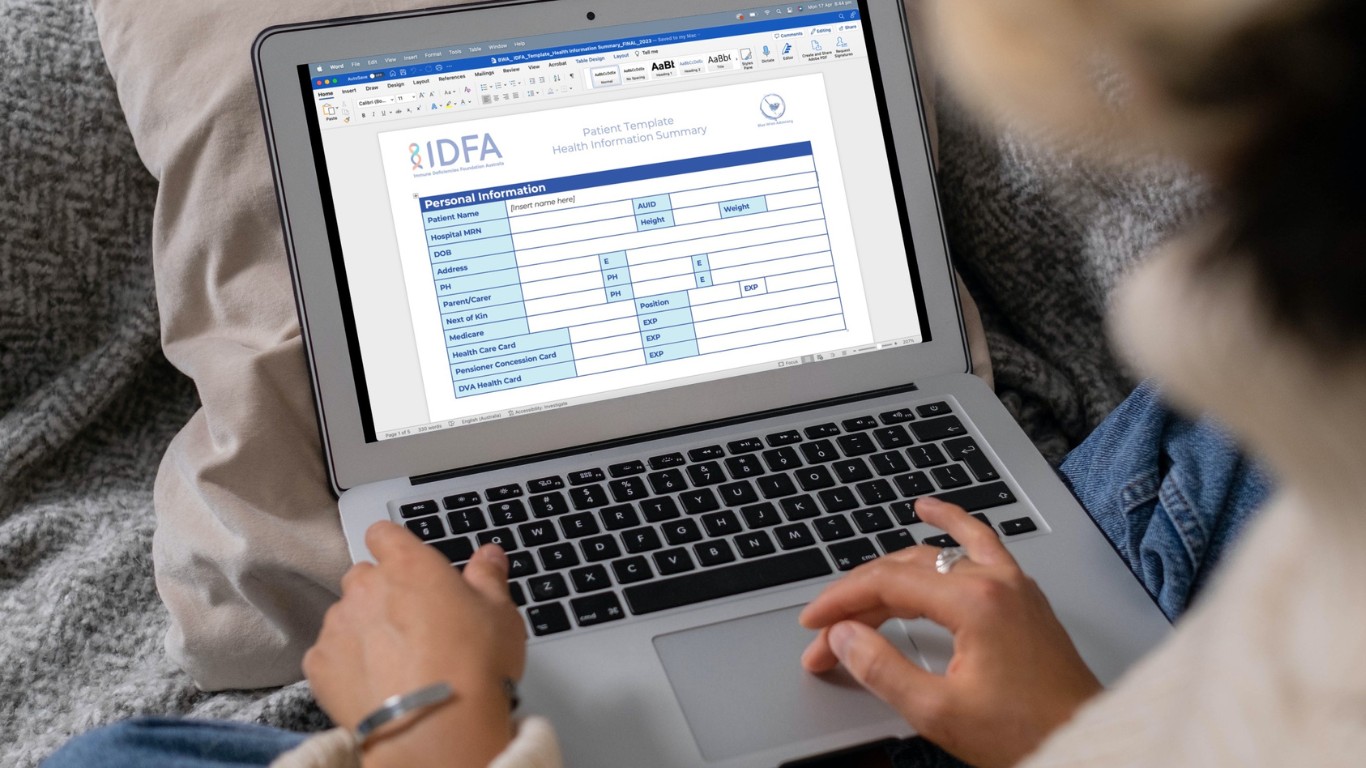
Self-Advocacy Toolkit
Tools to help individuals communicate with healthcare professionals, understand their diagnosis and treatment options, and make informed decisions about their health.